Alzheimer’s disease (AD) is a progressive and ultimately fatal neurodegenerative disorder. It is the most common form of dementia, accounting for 50-80% of all cases.
Late-onset AD, which strikes when individuals are in their 60s or older, is the most regular kind, occurring in 95% of all diagnoses. Early onset, or familial AD, which occurs when people are in their 40s or 50s, is rare and caused by mutations in the amyloid precursor protein, presenilin-1 or presenilin-2 genes. The cause of the more common form of the disorder, late-onset AD, is not known. Age is the strongest risk factor, with diagnosis of AD doubling every five years after the age of 65.
In the US, approximately one in eight adults aged 65 years suffers from AD; that number approaches one in two by 85 years of age. With the aging of the worldwide population, the global frequency of the disease is rising rapidly. The ‘World Alzheimer Report 2009’ estimated that 36 million people suffer from dementia globally and projected that the number of affected individuals would double every 20 years, reaching 115 million by 2050. All regions of the world are facing this looming epidemic, with an estimated 40% increase in those suffering from dementia between 2010 and 2050 in Europe, 89% in the Americas, 107% in Asia, and 111% in Africa.
The importance of early detection
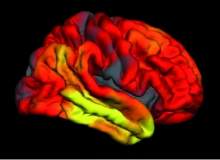
Currently, AD is diagnosed clinically only after the onset of dementia, when significant, widespread neuronal degeneration has occurred (Figure 1, below). Recent advances in biomarkers for early detection of the disease have made it clear that AD pathology begins to accumulate in the brain years before the onset of dementia. This provides the opportunity to detect AD at an earlier stage, prior to the start of functional decline. Although no treatments yet exist that can prevent or delay the course of the disease, early identification of the disorder is important for ensuring optimal care and aiding the search for treatments.
In the care setting, improved ability to identify AD in the earlier stage can help in differential diagnosis. A variety of conditions, many of which are treatable, can result in impaired memory and cognitive dysfunction in older patients. Accurate identification of the underlying cause of the impairment is necessary to ensure that patients receive appropriate treatment.
When evidence points to AD as the aetiology, early diagnosis can ensure that patients and carers are provided with appropriate information and support, as well as patients being prescribed the right medication. Although this will not alter the course of the disease, the report indicated that adequate support for carers can reduce stress; and this, combined with the symptomatic relief from current treatments, may delay the sufferer going into care and improve the quality of life for the patient and the carer alike. Early diagnosis also empowers patients to take an active role in planning their future and they may then choose to participate in clinical trials.
Accurate identification in the early stages of the disease is vital in the search for effective treatments. The lack of progress in recent studies has led to a consensus among researchers that to be effective, treatments must be administered early, before irreversible brain damage has occurred. This requires identifying participants for clinical trials who are in the early stage of the disorder and likely to develop dementia during the course of the trial if left untreated.
Those with mild cognitive impairment (MCI) are at an increased risk of developing AD and seen as a suitable subject for studies. Those with MCI have a 15-20% risk of developing dementia within a year, compared with a 1-2% risk for older people without cognitive impairment. Despite this increased risk, not everyone with MCI will go on to develop dementia. Cognitive impairment can arise from a variety of conditions, many of which can be treated; so additional information is needed to help determine an MCI patient’s risk of developing dementia.
The role of volumetric MRI in detection
A significant amount of research has shown that structural magnetic resonance imaging (MRI) is sensitive to the neurodegeneration associated with AD; even in the very early stages it can be used to determine someone’s risk of developing dementia. However, MRI is not routinely used to diagnose AD in clinical practice and the definitive diagnosis of the disease can only be made during an autopsy. During life, a clinical diagnosis of possible, or probable, Alzheimer’s disease is based on evidence of progressive memory impairment and functional decline, as well as the lack of evidence of any other cause of the impairment. As a result, the diagnosis is arrived at through a process of exclusion rather than on the basis of supportive findings. MRI, when used, is performed to rule out other causes of impairment, such as subdural haematoma and cerebrovascular pathology. Recent technological advances in volumetric MRI (vMRI) have set the stage for its use to provide supportive evidence for the diagnosis of AD. Advances in knowledge of the long prodromal phase of the disorder now allow for clinical detection prior to the onset of dementia.
AD is linked to the atrophy of parts of the brain associated with memory, particularly the hippocampus. This wastage is visible on high-resolution MRIs and simple visual ratings of the degree of decay can be useful in detecting neurodegeneration. However, it can be difficult to distinguish normal age-related atrophy from that associated with AD, particularly at the earliest stages of the disease.
Quantitative methods are necessary, which allow for comparison with normative data. Early work on quantifying atrophy in AD relied on the manual tracing of the hippocampus, slice by slice, on a 3D T1-weighted volumetric brain scan. These ground-breaking studies showed that AD is associated with the shrinkage of the hippocampus; and that individuals who suffer from mild cognitive impairment also show significant wastage of hippocampal tissue. Importantly, they demonstrated that both the degree of degradation from a vMRI obtained at a single point in time and the rate of change from serial vMRIs obtained one or two years apart predict progression of MCI to dementia.
The development of standardised image acquisition procedures and automated image analysis algorithms allows the translation of these research findings into the clinical setting. Although clinical MRI scans can be used to rule out other causes of impairment in suspected AD cases, they are not suitable for use in automated volumetric analyses.
The process explained
Recently, our group used a clinically available, automated MRI analysis method applied to data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) to demonstrate the ability of vMRI to predict the development of dementia in patients with MCI. This FDA-cleared image analysis software provides raw volumes of brain structures affected by AD, and compares the patient’s regional brain volumes with those of a normative database, correcting for gender, head size, and age (Figure 2). We used this software to calculate the medial temporal lobe atrophy in 192 of the MCI participants.
We quantified medial temporal lobe volume as the ratio of the volumes of the hippocampal to the inferior lateral ventricle. As the hippocampus shrinks with advancing disease, the ventricles expand to take up the space formerly occupied by its tissue, providing a measure of medial temporal lobe atrophy that is more sensitive to AD than hippocampal atrophy alone. We corrected this wastage measure for head size, sex and age, using ADNI’s healthy control population as the normative sample. We then split the MCI subjects into two groups, those showing normal medial temporal volumes – within one standard deviation of control group volume – and the other showing a smaller medial temporal lobe volume than expected for the patient’s sex, age and head size – more than one standard deviation below the normative group. The results were significant; they showed that participants with medial temporal lobe atrophy were at much greater risk of developing AD within three years. 75% of participants with medial temporal lobe atrophy developed AD by the end of the third year follow-up period, compared with only 30% of people without it.
In addition, people with medial temporal atrophy progressed to dementia at a rapid rate, with an average dementia-free period of just 15 months (Figure 3, left). These findings demonstrate the value of vMRI for identifying those most likely to suffer from prodromal AD and develop dementia in the imminent future.
Conclusions
vMRI is likely to become an important tool for assisting diagnosis in clinical settings where multiple causes may underlie a patient’s memory complaints. In cases where the clinical impression points to a neurodegenerative illness, vMRI can provide objective and direct supportive evidence of such neurodegeneration, allowing the physician to provide appropriate warning in advance to the patient and family, with stronger justification for pursuing a more aggressive course of intervention. Currently, this might include social, financial and safety planning, as well as training for carers and the potential recommendation for enrolment in clinical trials. In other cases where AD is suspected, vMRI results may show minimal medial temporal atrophy; this may prompt a more thorough investigation for other, potentially treatable causes of the impairment. With the aging of the worldwide population, AD is a growing public health concern that could have disastrous consequences on societies. It is vital that treatments are developed to stop or delay the course of this devastating illness.
The ability to detect AD early will aid in the search for effective therapies; when these are available, it will be critical for risk and benefit assessments to determine the treatment.
At the moment, early detection enables patients and families to access support services and symptomatic treatments at an earlier stage in the disease, which may reduce stress and enhance the quality of life.

This article was first published in our sister publication Medical Imaging Technology.



